Author: Daniella Marchick
How to Cope with Caregiver Burnout
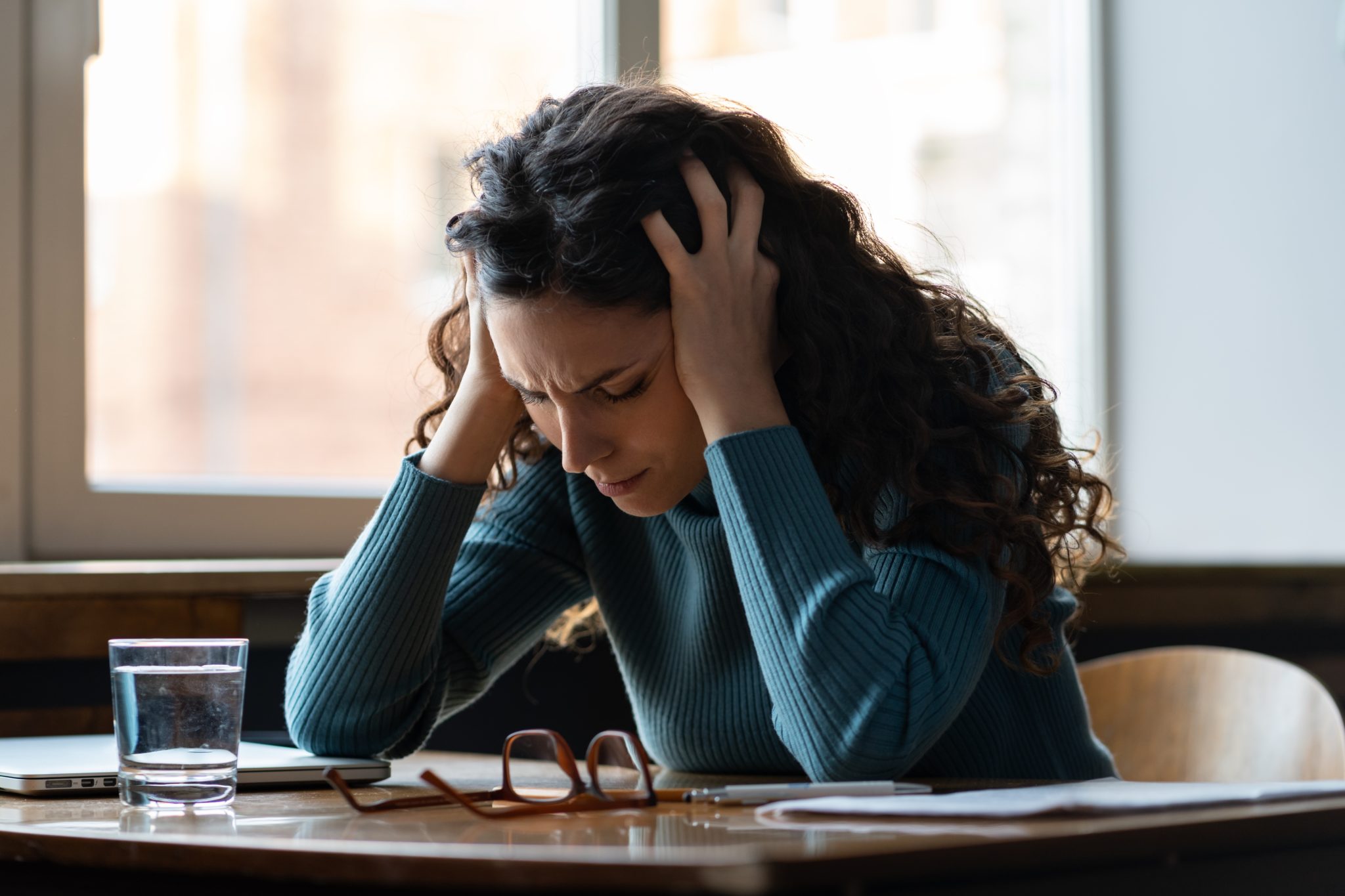
While taking care of a loved one may have its rewarding moments, it can also feel absolutely thankless and full of unexpected stressors. Sometimes you are so focused on providing care that it becomes hard to prioritize your own, as caregiving demands can turn out to be exhausting and even crushing at times. Because of this, it’s not uncommon to begin feeling powerless, depressed, and burned out.
According to WebMD, caregiver burnout refers to a state of physical, emotional, and mental exhaustion. Signs of caregiver burnout may include:
- Difficulty concentrating and making decisions.
- Intense and recurrent feelings of anger, sadness, or fear.
- Trouble sleeping.
- Drastic weight changes or other unexplained health problems.
- A noticeable difference in your ability to be patient, kind, or calm.
- Decreased participation in activities that bring you joy, like spending time with friends, activities, hobbies, maintaining relationships, etc.
Many caregivers spend an average of 20 hours per week caring for their loved ones. In addition to this, many are also working full-time (61 percent in 2020, reported by AARP) and possibly raising children too. Working while managing your caregiving responsibilities such as grocery shopping, picking up medications, transportation, and housekeeping can be overwhelming. Add in physical care as well, like bathing and helping with the toilet, it makes sense for one to feel overwhelmed. The tasks are a lot to take on, even if you’re sharing caregiving responsibilities with siblings or other family members.
Statistics show that caregivers report fair to poor health, which rises from 14 percent in the first year to 20 percent after 5 years or more. It’s extremely easy to fall into this state when you end up having to meet roles you didn’t anticipate, or when circumstances change.
The Family Caregiver Alliance indicates that caregiving can have somber physical health effects. In fact, 17 percent of caregivers feel their health, in general, has worsened as an outcome of their caregiving duties. Eleven percent of family caregivers say that caregiving has caused their physical health to worsen. Unfortunately, 40 – 70 percent of family caregivers have substantial clinical signs of depression-and caregivers report experiencing physical and emotional strain, even more so for those caring for loved ones suffering from Alzheimer’s and dementia (28 percent and 23 percent, respectively).
It’s important to stay on top of your own health to avoid burnout. Here are some ways you can find more balance in your role as a caregiver.
Ask for Help
Caregiving is a marathon. This is why asking for help can make a world of difference, both for your own mental health and the safety of your loved one. According to AgingCare, asking for caregiving assistance will help with managing the moving parts and avoid getting too stressed, anxious, and depressed. Ask yourself, “what can be outsourced and to whom?” Then, enlist the help of neighbors, friends, and family members. Create a schedule that allows for planned visits, check-ins, support; having your go-to support system in place when you need a break.
Join a Caregiving Support Group
Periodically surrounding yourself with others who completely understand your experience as a caregiver, and can support you in ways that others may not know how, is very valuable. A caregiver support group can provide a safe and comfortable space for you to talk about the challenges or struggles you may be experiencing. It can also be nice and even rewarding to help others too. Perhaps you’ll meet someone in the group who is now at a place where you once were, and you can give them the support and advice you wish you received at that time.
Enact Self-Appreciation
As hard as it may seem at times, practicing acceptance of your loved one’s conditions, and the role you’re playing in their care, can help uplift and empower you. Embracing your caregiving role and that you made a thoughtful choice to support them is powerful. Try celebrating small achievements within this role by reminding yourself that your efforts matter and you’re providing a quality of life to your loved one that others may not be fortunate enough to have. Research shows that appreciation (both external and self-driven) leads to greater physical and mental health in the face of the many demands of caregiving.
Seek Therapy With Someone Who Specializes in Caregiving
Prioritizing your mental health is critical as a caregiver. If you get too stressed, burned out, or depressed then you won’t be able to help anyone. In order to maintain stability and consistency in showing up for your loved ones, try seeing a therapist who specializes in supporting caregivers. A specialized therapist can help you with practical coping strategies, stress-relief tactics; getting good sleep, and generally being able to better manage your emotions and avoid caregiver burnout.
Remember, you cannot provide care for your loved one if you yourself are not physically, emotionally, and mentally fit for you first. Visit my website to learn more about caregiving and how to cope with caregiver burnout: https://marchickcounseling.com/services

Tips for Long-Distance Caregiving
Whether it’s a sick parent, an elderly family member, an aging sibling, or a dear friend in need, caregiving can feel like an overwhelming responsibility—especially if you’re having to help from a distance. According to the National Institute on Caregiving, a long-distance caregiver is an individual who lives one hour or more away from their loved one.
You’re not alone. The number of people becoming caregivers has increased over the years. In fact, “…over 34 million adults [in the US] are serving as a caregiver for a senior,” according to a study by The National Alliance for Caregiving. This number is going to dramatically increase as the baby boomers age.
Statistically, the majority of primary caregivers are women in their late forties to early fifties; 85 percent of which are providing care for a parent or parent-in-law.
Some of the tasks that a long-distance caregiver can assist with are the following: managing finances, scheduling appointments, dealing with insurance, communicating to other family or community members, and supporting primary caregivers through respite breaks. Other helpful things can include helping with legal needs, ordering things online, and connecting with your loved one frequently.
According to The National Alliance for Caregiving, around 15 percent (or 5 million) of caregivers live more than an hour away from the person they’re caring for—a number that’s expected to continue to grow.
Additionally, it’s very common for caregivers to spend their own money on care-related costs (things like travel to and from their loved one, groceries, and paid help) A. 2016 AARP study found that family caregivers spent an average of nearly $7,000 a year of their own money—more than $7,400 in 2019. That spiked to nearly $12,000 – $12,700 when adjusted for inflation—for caregivers who lived an hour or more from the care recipient. Costs generally were slightly higher if those receiving the care were 50 or older.”
Due to all of these responsibilities and expectations, it’s no surprise that caregivers are experiencing stress, anxiety, and grief. The National Alliance for Caregiving and AARP have found that 47 percent of long-distance caregivers report emotional distress, as compared to those who live less than an hour away (28 percent). As a long-distance caregiver, it is natural to experience a range of emotions including guilt, sorrow, anger, and anxiety. Working with a therapist like myself is a helpful way to feel supported during your time as a caregiver.
As a long-distance caregiver, it’s easy to focus on what you can’t control—the progression of the disease, for example. Instead, let’s talk about ways you can help reduce your own stress while ensuring your loved one is set up in the best possible way, from afar.
Setup Your Foundation
The first thing you may wish to establish is an emergency plan. Have it written down and posted somewhere in your home and in your loved one’s home, with the steps to be taken should an emergency arise. This may include ensuring someone local can get into the home (is there a spare key hidden somewhere?), having essential paperwork completed and accessible. Be sure to include your name, the name of your loved one, important contact information, and a direct line to the local hospital or ER.
If you haven’t already discussed money management, you may wish to request access (or help them set up and use online banking, as well as, to monitor for scams) so they can benefit from automated services—like scheduled food delivery, reliable weekly house cleaning, and medication refills.
Establish a Local Team
Having a small, trustworthy group of people, who are already located closer to your loved one, is a great way to ensure there is support if an issue arises.
Your team may include neighbors, nearby extended family members, a home care company, a financial planner, a therapist, a pharmacist, and primary physician; a food delivery service, and a home care cleaning.
Have a Communication Plan
As you’re deciding frequency and the method of things like visits, phone calls, emails, video chats, etc. it’s also a great time to consider incorporating other forms of technology as well. Think of daily essentials that will make it as easy as possible for you to keep in touch. From afar, you can also work with your friends and family to set up a schedule to keep your loved ones in contact with others, as well, to help provide a watchful eye.
You and your loved one may wish to install in-home monitoring systems, outdoor motion sensors, activity tracking devices (like a FitBit), and automatic pill dispensers. Also, consider what installments into one’s home are needed to keep your loved one safe, such as grab bars. Use technology to your advantage if your loved one is able to do so, but remember if it brings more frustration or stress to either one of you than it is worth, then traditional phone calls are still suitable.
Take Care of Yourself Too
Finally, it’s critical that caregivers prioritize their own mental and physical health as well! Caregiving is often long and unpredictable, you being at your best will help you make calm and rational decisions. It’s no secret that caregiving can be a stressful and often a very emotionally taxing experience.
To maintain your mental health it’s best to work with a therapist who is knowledgeable in caregiving, grief, death, dying, and loss. A therapist in this field can be great for helping with both practical decision making and processing emotions.
It would be an honor to work with you. To learn more visit: https://marchickcounseling.com/services
—

Educational Support Group Starting April!
Adults Caring for Aging Parents
Join fellow caregivers for a 6 week educational support group! Each week a different topic will be presented followed by a chance to provide each other with encouragement, comfort, and lived experiences.
The following topics will be addressed:
Week 1: Introductions & Understanding Caregiving
Week 2: Creating Teams, Clarifying Roles & Engaging Family Members
Week 3: Financial, Legal & Medical Permissions and Steps Involved
Week 4: Self-Care & Dealing with Difficult Behaviors
Week 5: Quantity & Quality of Life
Week 6: Anticipatory Grief & Death
Reach out to Daniella at marchickdaniella@gmail.com or 503-683-3179 for more information and to sign up.
Two support groups starting in April. Mondays 11 am April 22 – June 3 at Encourpreneuercafe in inner Northeast Portland. Tuesdays April 30 – June 4 at 7pm at Mindtree Holistic Counseling in Southwest Portland. A 6 week commitment is encouraged! $130 in advance or $25 each session.

Counseling for Caregivers
While caregiving, it is often hard to find time for oneself but it is essential to combat caregiver burnout.
Caregiving involves hardwork and dedication day in and day out. According to AARP’s National Alliance for Caregiving (2015) family caregivers spend an average of 24.4 hours per week providing care. Nearly 1 in 4 caregivers spends 41 hours or more per week providing care.
The responsibility of caring for a loved one may make people feel trapped in their role. Caregiving is mentally and physically exhausting and can lead to a variety of challenging feelings and increase physical symptoms of ailments.
Counseling can provide a non-judgmental outlet to express feelings of guilt, sadness, and anxiety.
Learning how to understand and address those feelings is one of the greatest benefits of counseling. Talking with a supportive individual can normalize the frustrations and sadness while being proactive in minimizing the burden and creating a healthy way to handle stress.
Being an overwhelmed caregiver may lead to feelings of isolation and powerlessness,. Understanding and addressing these feelings is one of the best ways to prevent caregiver burnout. Those who receive regular emotional support are better equipped to prevent burnout, handle difficult care decisions and balance their own needs with those of their loved ones.
With the help of Daniella, of Marchick Counseling, together we can tackle the burden of caregiving and the emotions that surround the often thankless task.
Together we can set up healthy patterns and boundaries that may help you care for your loved one for a longer period of time without becoming burnt out. Those who receive regular emotional support are better equipped to prevent burnout, handle difficult care decisions and balance their own needs with those of their loved ones.

Social Isolation
Often being socially isolated is correlated with feelings of being alone.
Social Isolation is an objective measure of the number of contacts or social connections. One may actively choose to not interact with others and not have feelings of loneliness. However, most often being socially isolated is correlated with feelings of being alone. According to Helen Beaman, MSW, whom is a part of Oregon’s Older Adult Behavioral Health Initiative, socially isolated older adults are likely to be sicker and die sooner, have higher health care expenses, and are more likely to need long-term care, than those who retain their social connections. Isolation can lead to pessimism about aging and increasing fears about the future. There are many socio-demographic risk factors that lead to social isolation with age being one of the main components.
Caregivers are also at high risk for social isolation.
As the individual whom they care for loses their ability to socialize, the caretaker also misses out on the opportunity to maintain social connections. It can be challenging to make plans ahead or get out of the house when your loved one is unpredictable with their needs or loses mobility. Sometimes feelings of embarrassment, anxiety or exhaustion from explaining to others diminishes the motivation to connect with loved ones.
Working with a therapist and attending a support group can help a caretaker address these feelings and associated challenges. At Marchick Counseling we can help you get back on the path of connection and develop strategies to guide you to a healthier and happier life. Call 503-683-3179 today to schedule an appointment.

Loneliness
At different stages in life, one may experience feelings of loneliness and/or isolation.
Though these concepts are often related, they are not one and the same. Loneliness is a feeling of not being as connected with others as desired. Loneliness can occur even while being surrounded by people. Robin Williams said “I used to think the worst thing in life was to end up all alone. It’s not. The worst thing in life is to end up surrounded by people who make you feel all alone.” According to a New York Times article, loneliness is most prevalent during teenage years, then again in the oldest old.
Individual and group therapy is a safe space to explore these feelings of loneliness.
Unfortunately, recent findings are correlating loneliness with earlier deaths, increased stress hormone cortisol, and is often a risk factor for depression. Perceived loneliness contributes to cognitive decline and is a risk for dementia. Often feelings of loneliness leads people to other behaviors such as unhealthy eating, smoking cigarettes, and lack of physical activity. Fixing loneliness is not as simple as surrounding oneself with others, it is important that these interactions provide a sense of meaning. Both individual and group therapy is a safe space to explore these feelings of loneliness.
At Marchick Counseling, together we can acknowledge these feelings are justified and create strategies towards healthy habits in reducing loneliness and creating meaning. Call 503-683-3179 today to schedule an appointment.
